年の瀬がせまり、あわただしい時期となりました。まだまだ女子医大オペ室も変わらず大忙しです。
そのような中、今年も12月14日に女子医大麻酔科忘年会がホテル椿山荘にて開催されました。
例年、当医局はホテル椿山荘で忘年会を行っていますが今年も大変盛り上がりました!!
各関連施設の先生方、医局員に限らずお世話になっている各方面の方々が大勢集まり、会場はいっぱいでした。また、参加者のお子様たちが遊べるお部屋も用意されており、ご家族そろって出席なさる先生方も大勢いらっしゃいました。このような配慮も女子医大ならではかなと。
まずは開会の言葉、尾崎教授。
各関連施設の先生方からお言葉。代表して写真はO病院A先生
そして、、毎年大好評の抽選会!
教授公認の一日休日券や
五万円の旅行券やルンバ、Kindle、ヨナナスメーカー、バリスタ、レイコップ…等今話題の家電もたくさん!当選者です。羨ましい!
そして、最後はこれまた毎年恒例の研修医と新入局員からの余興です。
麻酔科ローテーション中の研修医たちが一生懸命練習して準備してくれたのは、、?
パラパラ!!
化粧もバッチリ。きまってました!
急な余興の振りにもかかわらず完璧な出し物で会場も掛け声が飛び交いとっても盛り上がりました。
そして新入局員からは動画とダンスの余興でした。
動画は医局員の写真を集めて貼り合わせ(約1000枚!!)、一枚の大きな写真を作るというものでした。
出来上がりは、、?
ダンスはキンタローで今年再復活したフライングゲット!
大成功?!でした。おそらく!
尾崎教授と1枚。ヨーロッパへ旅立たれた野村教授がいらっしゃらないのが残念。
さて、今年もあとわずか。
錬士1年目としては今年は経験も知識もいっぱい積むことができ大変充実した1年間でした。諸先生方に大変お世話になりご迷惑もおかけ致しましたが、来年後輩が入局するということもありさらに飛躍できるよう努力してまいりますので引き続きよろしくお願い申し上げます。
それではよいクリスマスとお正月をお迎えください。
錬士Hでした。
2013年12月24日火曜日
Cell - Declining NAD+ Induces a Pseudohypoxic State Disrupting Nuclear-Mitochondrial Communication during Aging
Cell - Declining NAD+ Induces a Pseudohypoxic State Disrupting Nuclear-Mitochondrial Communication during Aging
老化に伴うNAD+低下は偽の低酸素状態を生み出し、核とミトコンドリア間連絡を妨げてミトコンドリア機能低下を招くが、
この現象は可逆的で、NAD+レベルを上げるとミトコンドリア機能が若返りうることがマウス実験で示された。
この研究のグループを率いるDavid Sinclair氏はNADを生み出す化合物を検討する会社Metrobiotech社を最近共同設立!
老化に伴うNAD+低下は偽の低酸素状態を生み出し、核とミトコンドリア間連絡を妨げてミトコンドリア機能低下を招くが、
この現象は可逆的で、NAD+レベルを上げるとミトコンドリア機能が若返りうることがマウス実験で示された。
この研究のグループを率いるDavid Sinclair氏はNADを生み出す化合物を検討する会社Metrobiotech社を最近共同設立!
2013年12月9日月曜日
錬士1年目の登竜門
すっかり冬らしくなり、肌寒い毎日が続いてきました。毎朝布団の誘惑に負けそうな毎日が続いている錬士Kです。
先月金沢で臨床麻酔学会が行われました。
今回はそのご報告をさせていただきます。
医局のご厚意により錬士1年目は日本麻酔科学会に全員参加させてもらえます。そこで偉大な先生方や先輩麻酔科医の素晴らしい発表を見学し、後に来る自分の番に備えます。そしてデビュー戦は秋にあるこの臨床麻酔学会になります。
今回は錬士1年目から4人が発表することができました。
1人目はT先生。
「メトクロプラミドを契機とした錐体外路症状を呈したと思われる周術期ドロペリドール投与例」初めてのポスター制作で悪戦苦闘されていましたが発表は堂々とされていました。
2人目はO先生。
「スガマデクス投与後に突如心静止をきたした症例」
使用頻度の高い薬の合併症についての内容で会場は興味深々という雰囲気でしたが、ホテルの自室にポスターを張り、ぎりぎりまで練習していた効果もあってか本番はビシッと決めていました。
3人目はK先生
「マッキントッシュ型喉頭鏡とビデオ喉頭鏡による気管挿管の生体力学的検討」発表は緊張でたどたどしかったですが視点が面白いと内容は好評でした。
4人目はO先生。他の3人はポスターでしたがO先生は徹底討論のセッションで発表されました。
「重症ASを合併した妊婦の帝王切開周術期管理」
症例は全身麻酔でやるか脊髄くも膜下麻酔でやるか大変難しいところで、討論は白熱していましたが堂々と受け答えされていました。
学会の後はもちろん…
指導してくださった先生方と金沢の料理を囲んで女子会
兼六園にてお茶を堪能。
このデビュー戦をみんな無事乗り越えることができました。
2013年12月8日日曜日
Ondansetron May Inhibit Analgesic Effect of Acetaminophen
Anesthesiology News - Ondansetron May Inhibit Analgesic Effect of Acetaminophen
Ondansetron May Inhibit Analgesic Effect of Acetaminophen
by Keely Savoie
Ondansetron may inhibit the analgesic effect of acetaminophen when the two drugs are co-administered, Canadian researchers have found. The recent study looked at children who received either ondansetron or droperidol in conjunction with acetaminophen during tonsillectomy surgery.
“Children who received the two drugs together needed more morphine in the recovery room after the operation,” said Pierre Beaulieu, MD, PhD, associate professor of anesthesiology and pharmacology at the University of Montreal. “Based on our findings, we think the co-administration of these two drugs is deleterious for pain relief.”
The researchers were scheduled to present their findings at the 2013 annual meeting of the Canadian Anesthesiologists’ Society (abstract 1652406), but the conference was cancelled because of severe flooding.
Dr. Beaulieu said his study confirms that acetaminophen and ondansetron engage the same serotonin (5-HT3) receptor. “Because acetaminophen and ondansetron are working on the same receptor, when they are administered together, there is a decrease in pain relief,” he said. Previous research demonstrated the inhibitory effect of ondansetron on acetaminophen in animal and human volunteer studies, but relevant clinical trials in humans had failed to show an effect.
Dr. Beaulieu and his colleagues designed a double-blind parallel group study of 69 children, ages 2 to 7, who underwent elective tonsillectomy and received acetaminophen as an analgesic. The researchers randomly assigned the patients to receive either ondansetron (n=35) or droperidol (n=34) as an antiemetic. The investigators assessed the children’s pain and morphine consumption for 48 hours after surgery.
There was no difference in postoperative nausea and vomiting (PONV) between the two groups, and the primary end point—postoperative pain—did not differ significantly between the two groups during the first 24 hours. Children who received ondansetron, however, were 2.8 times more likely to require morphine (57.1% vs. 20.6%). The amount of morphine administered to the ondansetron group was nearly three times more (279.5 vs. 97.6 mcg) than to children who received droperidol (Figure).
Dr. Beaulieu’s conclusions, however, are controversial. Sergio Bergese, MD, chief of neuroanesthesia at Ohio State University, in Columbus, and Suren Soghomonyan, MD, PhD, a research scientist at Ohio State, noted that the study did not include factorial controls, and therefore could not demonstrate a clear interaction. “Increasing numbers of patients receive acetaminophen and ondansetron in combination postoperatively to treat pain and reduce the incidence of PONV. Undoubtedly, clinically important interaction between those drugs, if any, would deserve further research and might have impact on clinical practice,” Dr. Bergese said. “However, in vitro, in vivo and clinical studies specifically designed to test the hypothesis of drug interaction are mandatory before making any conclusions. Any single clinical trial, especially when underpowered in regard of the specific objective, will be inconclusive.”
Furthermore, he stated, droperidol is a sedative and increases opioid effects, which would decrease total opioid consumption. The study may have been further complicated by the nurses’ interpretation of the patients’ need for additional morphine. “The sedative effect of droperidol could easily influence the nurses’ perception of patient pain,” he said.
Dr. Bergese also pointed out that acetaminophen may act on the 5-HT mechanisms primarily via the 5-HT7 receptors, whereas ondansetron is a selective 5-HT3 antagonist. In addition, endocannabinoid and opioid systems are major components of the antinociceptive activity of acetaminophen—and these systems are not engaged by ondansetron. “The overall picture in a clinical setting is more complex,” Dr. Bergese said. “Attempts to explain the cumulative effects of two drugs based on the assumption that these drugs interact on a single receptor level is over-simplification.”
For Dr. Beaulieu, the question is not settled. “We now need to design a large-scale study, ideally multicenter, to determine whether there is an interaction in a larger population,” he said. “If we confirm the interaction, we should change our practice and not give the two drugs together, and that will affect millions of people around the world undergoing surgery.”
“Children who received the two drugs together needed more morphine in the recovery room after the operation,” said Pierre Beaulieu, MD, PhD, associate professor of anesthesiology and pharmacology at the University of Montreal. “Based on our findings, we think the co-administration of these two drugs is deleterious for pain relief.”
The researchers were scheduled to present their findings at the 2013 annual meeting of the Canadian Anesthesiologists’ Society (abstract 1652406), but the conference was cancelled because of severe flooding.
Dr. Beaulieu said his study confirms that acetaminophen and ondansetron engage the same serotonin (5-HT3) receptor. “Because acetaminophen and ondansetron are working on the same receptor, when they are administered together, there is a decrease in pain relief,” he said. Previous research demonstrated the inhibitory effect of ondansetron on acetaminophen in animal and human volunteer studies, but relevant clinical trials in humans had failed to show an effect.
Dr. Beaulieu and his colleagues designed a double-blind parallel group study of 69 children, ages 2 to 7, who underwent elective tonsillectomy and received acetaminophen as an analgesic. The researchers randomly assigned the patients to receive either ondansetron (n=35) or droperidol (n=34) as an antiemetic. The investigators assessed the children’s pain and morphine consumption for 48 hours after surgery.
There was no difference in postoperative nausea and vomiting (PONV) between the two groups, and the primary end point—postoperative pain—did not differ significantly between the two groups during the first 24 hours. Children who received ondansetron, however, were 2.8 times more likely to require morphine (57.1% vs. 20.6%). The amount of morphine administered to the ondansetron group was nearly three times more (279.5 vs. 97.6 mcg) than to children who received droperidol (Figure).
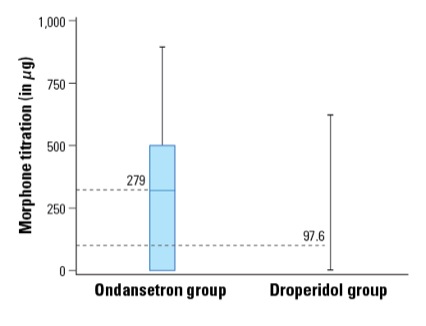 Figure. Morphine titration in the recovery room expressed as median and interquartile range (box) (P=0.01) |
Furthermore, he stated, droperidol is a sedative and increases opioid effects, which would decrease total opioid consumption. The study may have been further complicated by the nurses’ interpretation of the patients’ need for additional morphine. “The sedative effect of droperidol could easily influence the nurses’ perception of patient pain,” he said.
Dr. Bergese also pointed out that acetaminophen may act on the 5-HT mechanisms primarily via the 5-HT7 receptors, whereas ondansetron is a selective 5-HT3 antagonist. In addition, endocannabinoid and opioid systems are major components of the antinociceptive activity of acetaminophen—and these systems are not engaged by ondansetron. “The overall picture in a clinical setting is more complex,” Dr. Bergese said. “Attempts to explain the cumulative effects of two drugs based on the assumption that these drugs interact on a single receptor level is over-simplification.”
For Dr. Beaulieu, the question is not settled. “We now need to design a large-scale study, ideally multicenter, to determine whether there is an interaction in a larger population,” he said. “If we confirm the interaction, we should change our practice and not give the two drugs together, and that will affect millions of people around the world undergoing surgery.”
2013年12月7日土曜日
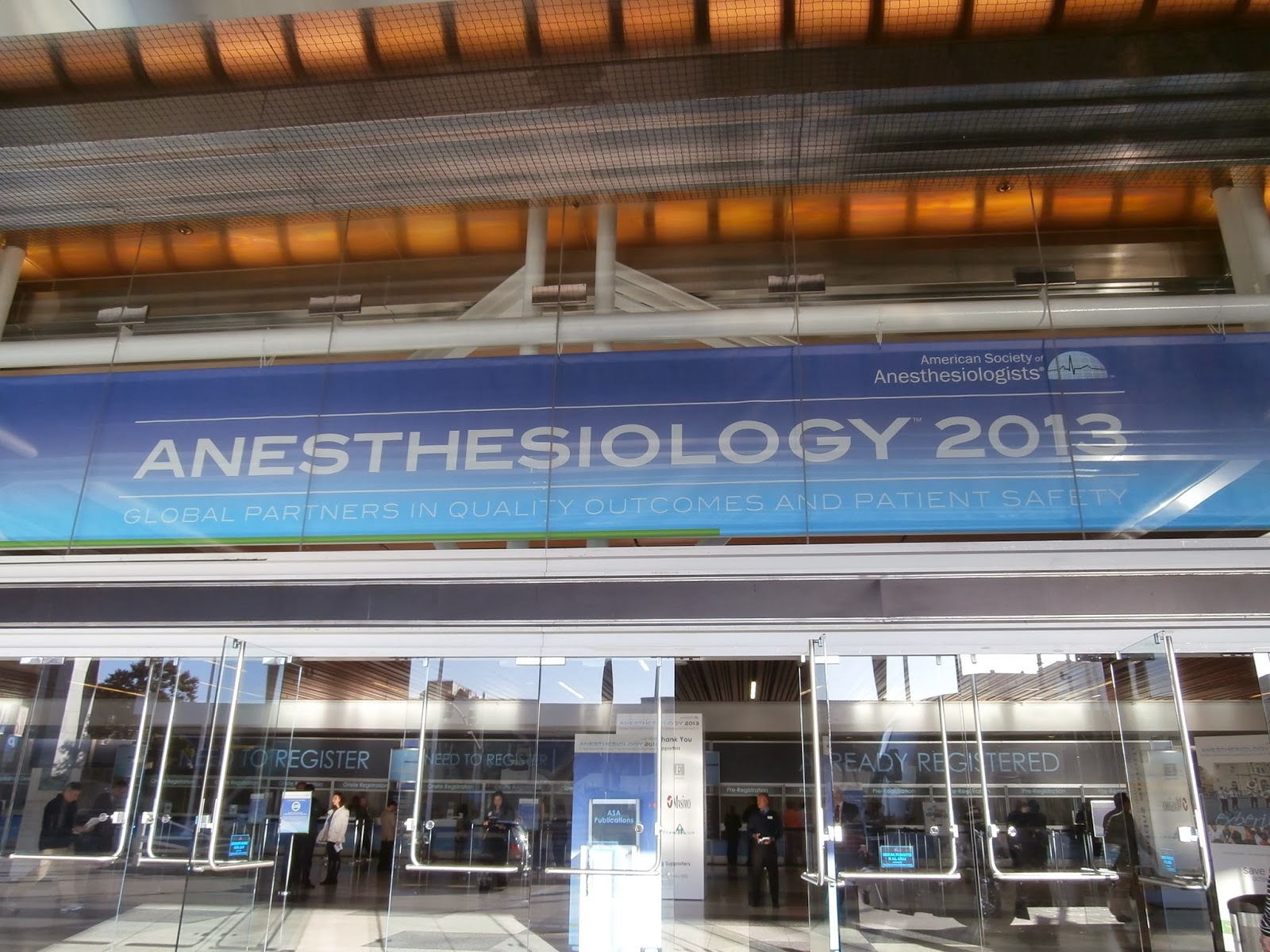
ASA@San Francisco
SDカードが読めない等々の諸事情により、だい~
ASA@San Francisco報告です。
日本から直行便のあるSan Francisco.
ケーブルカー、ゴールデンゲートブリッジの街で、
会場はとってーも広くて、歩くだけで疲れました。
日本からの参加者も多く、
当科からは5演題。
ポスターセッションでは今年からe-
会場のモニターに映されました。
・・・予想以上に見にくい・・・
1セッション8演題でモニターは4つ。
2順目の私は自分のポスターがどう映るかが直前までわからずドキ
語学の高い壁に加えてこんな心配もしました。
最終日はリフレッシャーコースです。
肺保護戦略のお話を聞きましたが、知ってる話題だというのに
耳に入ってくるのは文章ではなく、単語のみ。。。
今度の書き初めは「英語の勉強!」に決定した瞬間でした。
ドキドキハラハラ以外に、楽しい時間も満喫。
当科からSan Francisco留学中のK先生はとっても元気!!
一瞬誰かわからないほどはじけてました。
カナダ留学中のN先生もASAにいらしていて、
お二人とも素敵でした。
なんとか時間をやりくりして、
ぶどう畑に癒やされ、美味しいワインにニヤニヤしっぱなし。
もちろんおみやげワインもゲット!!
密度の濃い数日間を過ごすことができました。
参加させてくださった医局の皆さま、ありがとうございました。
ASA@San Francisco報告です。
日本から直行便のあるSan Francisco.
ケーブルカー、ゴールデンゲートブリッジの街で、
会場はとってーも広くて、歩くだけで疲れました。
日本からの参加者も多く、
当科からは5演題。
ポスターセッションでは今年からe-
会場のモニターに映されました。
・・・予想以上に見にくい・・・
1セッション8演題でモニターは4つ。
2順目の私は自分のポスターがどう映るかが直前までわからずドキ
語学の高い壁に加えてこんな心配もしました。
最終日はリフレッシャーコースです。
肺保護戦略のお話を聞きましたが、知ってる話題だというのに
耳に入ってくるのは文章ではなく、単語のみ。。。
今度の書き初めは「英語の勉強!」に決定した瞬間でした。
ドキドキハラハラ以外に、楽しい時間も満喫。
当科からSan Francisco留学中のK先生はとっても元気!!
一瞬誰かわからないほどはじけてました。
カナダ留学中のN先生もASAにいらしていて、
お二人とも素敵でした。
なんとか時間をやりくりして、
ぶどう畑に癒やされ、美味しいワインにニヤニヤしっぱなし。
もちろんおみやげワインもゲット!!
密度の濃い数日間を過ごすことができました。
参加させてくださった医局の皆さま、ありがとうございました。
2013年12月1日日曜日
日本麻酔・集中治療テクノロジー学会
日本麻酔・集中治療テクノロジー学会に参加して参りました。
第31回のテーマは、”他分野のテクノロジーに学ぶ”というカッコイイタイトルです。
今年の会場は東京国際フォーラム@有楽町でしたので、朝イチのセッションでの発表でしたが、
私はこの学会には初参加でしたが、噂にたがわぬ名物先生方(
正直、高度すぎてさっぱりわからないご発表もありました…(
今回はテーマが「他分野の」となっていたため、麻酔・集中治療領域のみならず、工学部、外科、呼吸器内科、
初参加ながら、充実の一日を過ごすことができました。
▲ 招待講演の座長の尾崎教授
登録:
投稿 (Atom)


















.jpg)

