・臨床研究の進め方
主題とは少しズレますが。。
とっても便利なビデオ喉頭鏡のこわ~いお話。まだまだ置いていない病院が多い中、当院中央オペ室ではマックグラス挿管時の第一選択になっています。
以下はマックグラスでの症例ではなく、他のビデオ喉頭鏡デバイスによる症例ですが
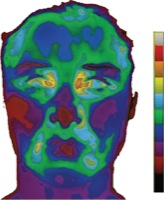
ビデオ喉頭鏡、「画面見ながら挿管できて楽ちん~♪」と、油断していると… ↓↓
↑こんな事態にもなります。わかりますか?気管チューブが軟口蓋(SP)を貫いてしまった事例です!!恐ろしや…。
今のところマックグラスではこうした症例はないものの、画面での挿管に頼りきっているとこうなるぞという勉強をしました。
**************************
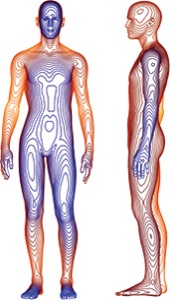
さて。では、気を取り直して、今中央病棟で使っているマックグラスの話に戻ります。パンフレットに載っている図がわかりやすいです。
上図のオレンジ色の部分がマックグラスの画面で見える部分、青色の部分が通常の喉頭鏡から見える部分です。実はマックグラスでは見えてない部分がこんなにあったんですね。
気管チューブが声門を通るまでは、マックグラスの画面に頼らず、自分の目で確認してから挿管するようにしましょうね。
・ICU報告会
1ヶ月間ICUローテートを終えた錬士1年目による報告会。
初めてのICU一人当直も、上級医の先生方のご指導で無事乗り切ったようです。
余談ですが、三連休最終日、錬士1年全員でバーベキューに行ってまいりました♪
麻酔中はオペ室でみんなバラバラだけど、こうして集まると気兼ねなく飲める同期って、素敵ですよね♪
これで今月もあと半分、がんばれそうです♪






 Research showing that more than 7% of thoracic surgery patients experience postoperative hypothermia despite active warming is raising questions about the appropriateness of current criteria for the hypothermia quality measure.
Research showing that more than 7% of thoracic surgery patients experience postoperative hypothermia despite active warming is raising questions about the appropriateness of current criteria for the hypothermia quality measure.