☆★――――――――――――――――――――――★☆
<日本臨床麻酔学会メールマガジン> 第11号
☆★――――――――――――――――――――――★☆
日本臨床麻酔学会から第11号(2013年11月号)メルマガのお届けです。
-------------------------------------------------------
I N D E X
●第33回大会印象記
●第34回大会の抱負
●日本臨床麻酔学会公認の臨床技能資格
!!
●学会賞獲得への道
●学会誌最新号から
-------------------------------------------------------
☆.。:・★.。:*・☆.。:*☆.。:*・★.。:*・☆.。☆.。:*・★.。:*・☆.。:*☆.。:*・★.。:*
■ 第33回大会印象記
第33回学術集会は、11月1日から3日間にわたり、金沢医科大学麻酔科学講座の
土田英昭教授の会長の下に金沢市で開催されました。11月の北陸とは思えない
晴れた暖かい天候に恵まれ、絶好の学会日和(勉強にも、観光にも)となりました。
学会のテーマである「和」を具現化するような大会で、会員相互の懇親の「和」や
日本情緒を満喫する「和」、基礎の成果を臨床に融合させる「和」、さらには
JALホテルとANAホテル、石川県立音楽堂を結んだ会場の「輪」を強く感じました。
斬新なアイデアも随所にみることができました。独立した部屋での同一テーマの
ポスター発表は、発表者や聴衆には好評でしたが、座長にはちょっと辛かったようです。
少ない演題数で、座長と聴衆の辛辣な質問に答える徹底討論は、反対に発表者には辛かった?
学会のプログラム内容に呼応するかのように、各会場とも盛況で熱心に討論されていたのが、
強く印象に残りました。
残念だったのは、会場の都合で機器展示が3カ所に分散していたことでした。
やはり、1カ所に纏まっていた方が、見学者には好都合のようです。
ちなみに私は、30分限定のティーブレイクに供された和菓子の味に感激しました。
-------------------------------------------------------
■ 第34回大会の抱負
第34回学術集会会長の東京女子医科大学麻酔科学講座主任教授である尾崎眞先生に、
次期大会のテーマと抱負をインタビューしました。テーマは、「ダイバーシティ」で
多方面に分岐して成長を続ける麻酔科学を表現すると共に、刺激的な自由な発想を
促進することも表現しています。金沢の「重厚さ」と対極にある東京の「軽快さ、爽快さ」
をイメージした学会運営を目指しています。会員の皆様の刺激的で自由な発想に基づいた
演題のご応募をお待ちいたしております。
-------------------------------------------------------
■ 日本臨床麻酔学会公認の臨床技能資格
!!
日本臨床麻酔学会でお馴染みのハンズオンセミナーへの参加で、超音波ガイド
下神経ブロックとDAMの臨床インストラクターの資格を獲得しましょう。
この制度に関し、来年の発足に向けて準備中です。
インストラクター申請受付についての詳細は、HP等で告知予定です。
-------------------------------------------------------
■ 学会賞獲得への道
日本臨床麻酔学会には、魅力的な学会賞が多数設けられています。
山田芳嗣学会賞選考委員会委員長に賞を獲得する「こつ」を伺いました。現在、賞への
応募数が少ないので、獲得するには「今でしょ」ということです。臨床に直結するような
基礎研究や目から鱗が落ちるような発想の臨床研究が、審査員にはぐっとくるようです。
学会最高賞の小坂二度見記念賞は、今後はIARS
(International Anesthesia
Research Society) の賞も兼ねる権威ある賞 (Kosaka Award)
になるようです。
現在研究を継続されている会員の方は、奮ってご応募下さい。
-------------------------------------------------------
■ 学会誌最新号から (編集室より)
「日本臨床麻酔学会誌」33巻7号の発行は近日、11月中旬です。
昨年の日本臨床麻酔学会
第32回大会(福島)の各講演、シンポジウム等の
特集や投稿論文(総説、原著、症例報告)などをラインナップしています。
学会誌33巻7号の目次はこちら⇒<
http://jsca.umin.jp/images/dl/pdf/vol33_noXXXXX.pdf>
-------------------------------------------------------
(広報委員会委員: 稲垣喜三)
/\/\/\/\/\/\/\/\/\/\/\/\/\/\/\
本メールマガジンの解除はこちらから
https://secure01.red.shared-server.net/www.waaint.co.jp/jsca_mm/==============================================================
【配信元】日本臨床麻酔学会
広報委員会
本メールにお心当たりのない方は、
お手数ですが<
mailto:jsca@waaint.co.jp>までご連絡下さい。
日本臨床麻酔学会
http://jsca.umin.jp/







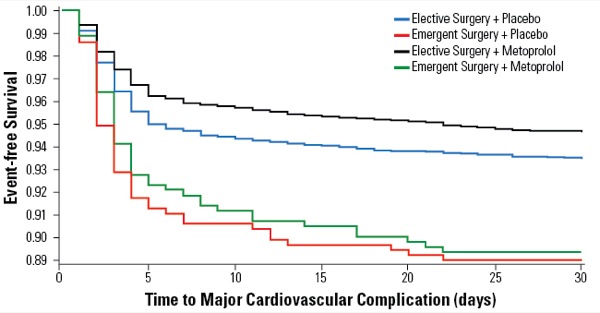
 The debate over using β-blockers perioperatively for non-cardiac surgery patients continues with a new meta-analysis from British researchers indicating that starting the drugs specifically for surgery can increase a patient’s risk for death by 27%.
The debate over using β-blockers perioperatively for non-cardiac surgery patients continues with a new meta-analysis from British researchers indicating that starting the drugs specifically for surgery can increase a patient’s risk for death by 27%.